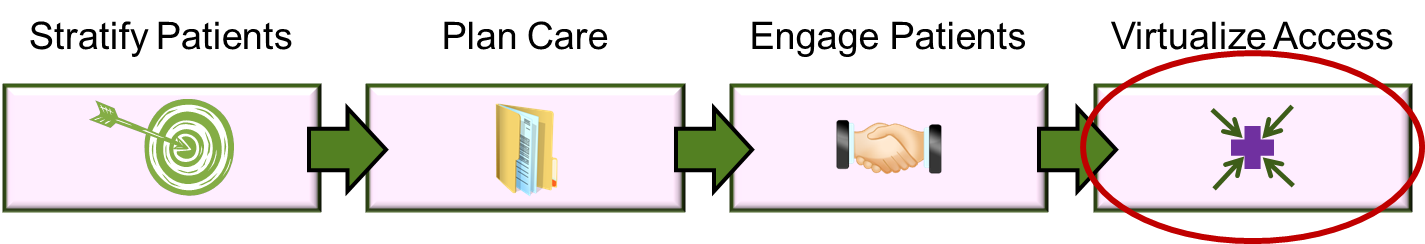
What is “Virtualized Access”?
We use “virtualized access” to mean exactly one thing:
- All participants in the plan of care can see (and act on) the same plan of care
By “participants” we mean all providers, the patient and the patient’s family. This is a slightly different statement than suggesting that all participants should be able to see the “chart” for the patient. For most patients, fragments of their chart exist in many places (that is, at each provider a patient visits). A “virtual chart” would integrate all of these chart fragments into a single uniform view of the entire chart. Virtual access to a chart is feasible, but rare. Unfortunately, virtual access to a common plan of care is even rarer. Some large integrated delivery systems have implemented multi-clinical-setting electronic medical record (EMR) systems that create an integrated view of the chart.
In those environments where all providers and patients are attached to a single medical group or provider system and that provider system has a broadly-installed EMR system and the patient portal gives patients access to the electronic chart, existing clinical systems might be able to support virtualized access to a plan of care.
But the EMR per se is only foundational to the next step: giving all participants (including the patient/family) access to the plan of care. The plan of care has to exist, and everyone who participates in it has to be able to see it. Most clinicians and patients do not have have access to such technology. And some categories of patients (particularly Medicaid and Medicare/Medicaid dual eligible patients) almost never have all of their providers in a single organization.
In most instances, patients move between separate provider organizations (technically, separate “PHI domains”) and this makes the technical solution a little more complicated.
Don’t HIEs solve this problem?
HIEs (Health Information Exchanges) were intended to solve a portion of this problem. However, most HIEs are (to be gentle) a little bit rudimentary in solving the clinical coordination problem. Some HIEs indeed enable access to some clinical data. To our knowledge, none of the classic HIEs enabled access to a common plan of care. The existing industry standards are a little behind supporting this function.
(FYI, we use the sort-of-standardized definition of “HIE” here: a tool set that provides access to “federated” data via centralized indexes and “edge” services for each data location. This definition excludes tools that centralize data. We also do not believe that large HIE clinical federated databases will ever be economically successful, but that is another story. The next-generation “HIE”s with centralized repositories are not truly HIEs in the classic sense. These are clinical data aggregators, and are far more useful and cost effective. The short story here is that classic HIEs are not particularly useful, but the newer clinical data aggregation tool sets are much more so.)
To be sure, the need for virtualized access to a common plan of care is not a rare problem. It is fairer to say it is a generalized problem in the industry. It has generally not been trumpeted as a significant issue because most providers are not accountable for care, and no one really wanted to bear the cost of the technology unless it was economically justified. But technology is not really the core problem.
Technology is not the problem?
As much as we enjoy chattering about technology and cool products, technology is indeed not the problem. It is technically feasible to implement and operate a secure, virtualized plan of care for about $5-15 per member per year. But if an organization is not going to deploy the care management processes to manage the costs of care down (which cost far more than the technology), the investment is not worth the expense. However, if the provider organization does indeed expect to implement the care management processes (e.g., stratification, care plan development, patient engagement), the technology costs are incidental.
More simple arithmetic
How can I contend that $5 to $15 per member per year is incidental? Consider the following example:
- Patient population: 100,000 members
- Average cost per patient (annual): $10,000 (this is probably reasonably close for 2014)
- Total population cost (annual): $1,000,000,000
- Care management cost reduction target (annual): 5-7% ($50 to $70 million)
- Care management process costs (annual): Approximately $10-15 million
- Portion of care management costs attributed to technology (assume $10 annual per patient): $1,000,000
Does it make a lot of sense to focus on getting the technology costs down? Wouldn’t it make more sense to focus on the cost reduction target or attempt to optimize the care management process costs?
If the clever, seductive logic above tickles your interest, you probably ought to call us.


