What is a “plan of care”?
For the purposes of this discussion, a plan of care is any set of interventions that are scheduled for a patient. Interventions are generally divided into:
- Medical interventions: These are the activities that are directly related to clinical state of a patient. Medical interventions could include tests, procedures, medications, therapies, or any activity that directly relates to medical diagnosis or treatment.
- Non-medical interventions: These are the activities that are are not directly related to medical care, but are required to make compliance with the medical plan of care more likely. Non-medical interventions would certainly include nursing interventions, and will also include interventions that may not be automatically associated with nursing activity. Examples beyond standardized nursing interventions (e.g., as standardized by NIC/NOC or Omaha, etc) may include arranging for transportation, training on care issues or nutrition, development of family support structure, or assistance with acquisition of safe, affordable housing.
Development of a patient-specific plan of care
There are many ways to describe the components of a plan of care, and many names to apply to each set of components. For the sake of this discussion, consider the following as a schematic of the process to create a plan of care:
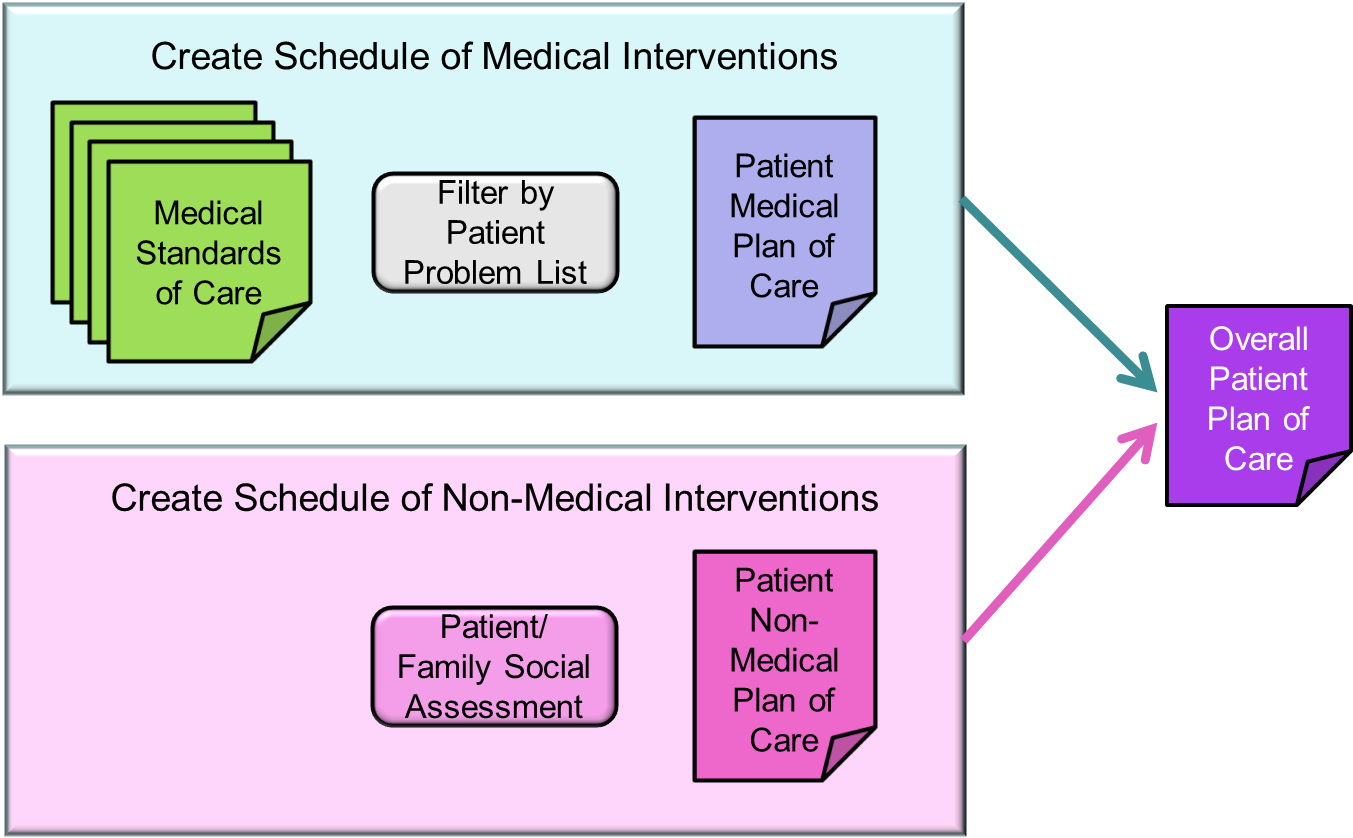
We have two groups of interventions, one medical and one non-medical. When merged we have an “overall” plan of care. The overall plan would have the universe of medical interventions required to address the patient’s medical issues (either to diagnose or treat) and all of the non-medical activities required to enable the patient to comply with the medical plan
Now what?
The art of care management is not in defining a plan of care. The art is in figuring out the “best” way to complete the plan (that is, to complete the interventions). In most contexts, the “best” approach is the least expensive avenue to complete the plan. The care team will usually opt for the least expensive approach for each intervention, or to substitute a single (expensive) intervention for a set of interventions that were inexpensive individually, but expensive in aggregate.
Often, the least expensive way to get interventions completed is to engage the patient and the patient’s family to assist. Clearly, the majority of medical interventions require a provider for delivery. But the majority of non-medical interventions do not require a provider, and can (and usually should) be leveraged onto the patient/family.
The less expensive, the better
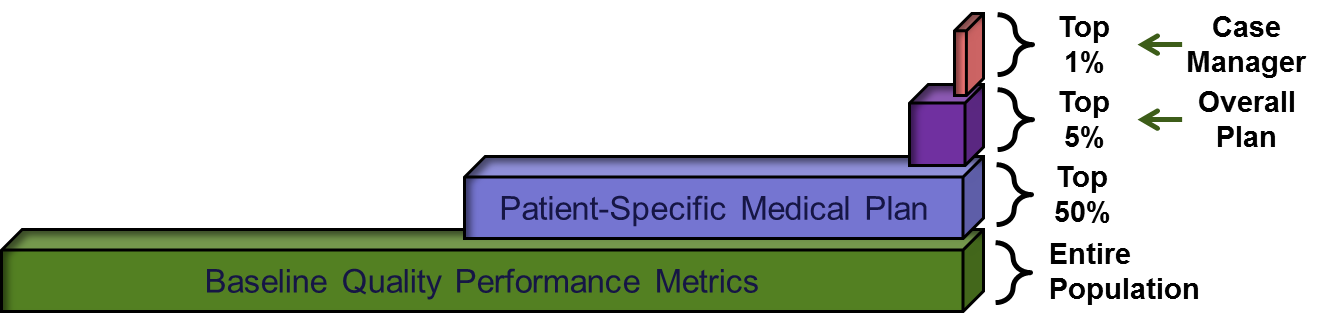
If we can get the cost of managing a plan of care down, the result is that we can increase the number of patients who are care management targets. If our only approach to care management is to assign a case manager to directly interact with patients, we are unlikely to get beyond the top 1.5% of patients with an active plan of care. On the other hand, if we can directly engage the patient and family to coordinate care, we are far more likely to be able to manage the 50% of dollars that are invested in the top 5% of patients.
Some quick arithmetic
If a population incurs an average cost of $10,000 each (which is probably about right for 2014), the top 1.5% is likely to be incurring well over $200,000 each. The next 3.5%, however, are likely approaching about $50,000 each. We have a lot of options to deploy services in this first population where annual care costs are very high and an investment in care coordination of $5,000 or $10,000 could easily pay for itself. We have fewer options in this second population where the cost of care coordination should likely be held to a range of $1,000 to $2,000 per patient per year.
The “purple problem”
In our view, identifying the best way to handle the second-most-expensive population is the middle of the problem. This set of folks is represented in purple below, and is the set of folks that are most likely to be transitioning to higher utilization. They are also probably the most challenging population to include in cost-effective care management services.
Process control systems
Generally, the techniques to manage completion of the plan of care require technology. This is particularly true for the population represented in purple above. Just as we used predictive modeling tools to identify the patients that are targets for plans of care, process control tools (as reflected in EMRs, centralized clinical data aggregates, clinical data interchange, etc) are required to manage the cost of coordination of the plan of care. This is discussed in more detail under “Engage Patients”:
Go to “Engage Patients”



