I am pleased by the frenzy of investment in tools that support the various elements of accountable care/population health. I am a little surprised how rarely the advertised tools are detailed by the business functions that the tools support. I would suggest there are three broad categories of tools in support of accountable care:
- Provider performance measurement
- Predictive analytics
- Care coordination
Each of these categories has one or more key subcategories. I think it would be useful to detail the subcategories to assist in IT tool selection.
Provider Performance Measurement Tools
This is the category that has been around the longest, and hence is the most mature. Typically, these tools aggregate claims and group the claims by care episode. Grouping of claims by episode gives an organization two fundamental capabilities:
- If the organization is going to contract for care, the tools give information on how to craft the contract, or indeed whether to contract at all
- If the tools are used during referral of an active patient, the tools can direct a clinician to select a referral target based on previous cost and quality performance
There are literally dozens of tools in this category. The problem for most provider organizations is gaining access to a significant fraction of claims history to run the tools. This is somewhat easier for a health plan (because they have the claims for their members) but a provider organization might need claims from multiple payers about many other providers to make this tool perform successfully.
Predictive analytics
Predictive analytics tools are used for two broad purposes as well:
- Prospective assessment of costs for a defined population to support actuarial assessment/pricing
- Identification of individuals likely to be utilizers to target treatment to mitigate the risk of adverse cost or quality events
The claims-based predictive analytics tools are quite good at supporting the first bullet above. Unfortunately, claims-based analytics tools are poor at the second. The two problems with claims-based tools are 1) the predictive value is low for individual patients (R-squared is often under 50%) and 2) the claims arrive too late to be of any use (60 days post discharge does not give a lot of insight).
Non-claims-based predictive tools are much more reliable if the objective is to direct active patient care. Non-claims-based tools would include:
- Tools to assess probability of readmission of a patient at discharge: This assessment is based on current clinical data (from the chart) and knowledge of the patient’s social circumstances (from interview or home assessment). This data, although harder to accrue and generally available only to the provider directly, is vastly more useful for predicting utilization.
- Tools to stratify populations based on global risk: Nearly any primary care physician can identify the top 3-4% of risky patients in his/her practice. Risk, in this context is a combination of overall disease burden and weakness of social support mechanisms (primarily family) for the patient. Patients with high disease burden could be targeted for a deeper home assessment to identify preventable risks or potential family support mechanisms to mitigate the risk of utilization.
It is worth noting that disease burden alone is often not a particularly strong indicator of future utilization, hence inclusion of data about a patient’s home environment is critical. The non-claims-based tools are often much more manual, but far more effective at identifying the high-utilization patients in advance.
There are many tools to assist in the prediction of population costs, and they work well. There are very few tools to assist a provider organization in identification of high-risk patients.
Care Coordination Tools
As with the other tools, there are two very different objectives in care coordination:
- Disease management tools: These tools establish clinical objectives by disease state for each patient to assist in filling in gaps in care and to support reporting of compliance standards to external entities (payers, CMS). Disease management tools support compliance reporting and quality management. They do not drive cost reduction (indeed, they often raise utilization).
- Case management tools: These tools focus on specific patients in high-risk categories to manage the risk of excessive utilization or risk of treatment failure in complex conditions.
There are many tools that support disease management functions. These may be a component of the EMR specific to the clinical setting, or an add-on application to the EMR. In contrast, case management tools are somewhat more rare in the marketplace. The problem, as often as not, is that the critical issues in case management are often inter-clinical-setting. The implementation problem may be large enough that the provider organization is not well situated to “connect” to all of the key clinical settings to enable effective case management.
A Note on HIEs
Some might consider HIEs as an element in care coordination. In my view, HIEs alone do not “count” as care coordination tools. They may (or may not) be supportive, but if a tool cannot instantiate an intervention and report on completion of an intervention, it is tough to label it as a care coordination tool. Most HIEs would fail in this regard.

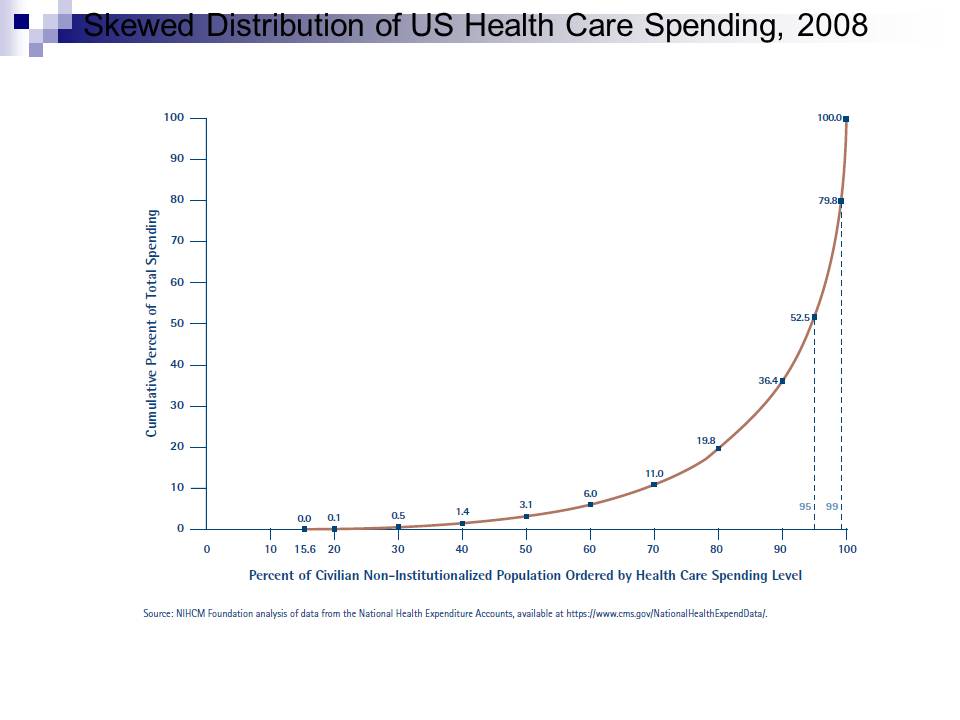 You can see that the graph shows the top 1% consume about 20.2% of care costs, and the top 5% consume about 47.5%. I think (but I am not sure) this is the overall US healthcare population (it sounds close).
You can see that the graph shows the top 1% consume about 20.2% of care costs, and the top 5% consume about 47.5%. I think (but I am not sure) this is the overall US healthcare population (it sounds close).
