Health plans versus provider organizations in “accountable care”
Much of the discussion related to accountable care is led by payers. Undeniably, the role of the payer is critical in that the payer must agree to changes in provider compensation to reward accountable behavior on the part of providers. In our humble view, this is the easy part. Some of the elements of provider payment are indeed complex, including:
- Global payment, capitation and subcapitation
- Share savings arrangements, and
- Risk corridor management, including stop losses for outliers.
However, none of these arrangements actually accrue any value unless provider organizations are able to reduce the costs of care for their “attributed” population. Given that health plans clearly have patients “attributed” to them too, why has health plan success in managing costs has been so muted?
(Authors note: we use the phrase “so muted” here because we have many highly skilled, hard-working colleagues in health plans. We could have substituted “a resounding failure”, but we did not want to discredit the heroic efforts of said colleagues.)
Experience suggests that implementing appropriate economic incentives is necessary but not sufficient to enable accountable care.
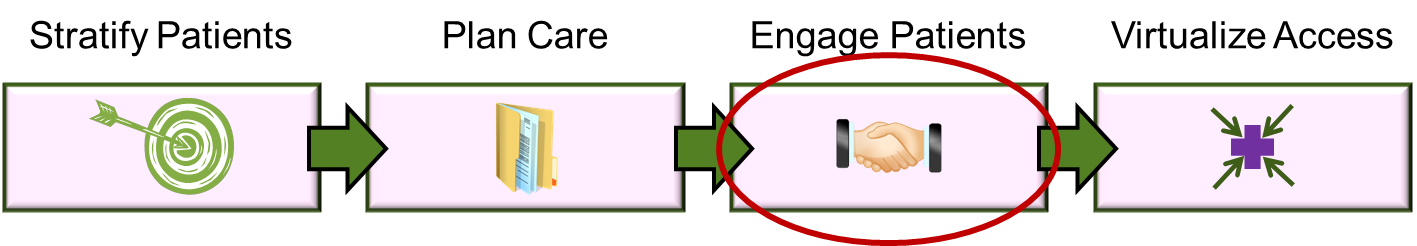
The critical value of patient engagement in reducing costs
The reason that provider organizations have far more capability to impact the cost of care is twofold:
- Providers make the majority of utilization decisions, and
- Providers have a far greater opportunity to engage the patient.
The latter is particularly important for the high-utilization target populations of interest. Payers often contend (correctly) that they have access to the patient and vice versa. Payers indeed typically maintain call centers to handle inbound service requests, and often maintain programs to assist members in managing disease issues.
But comparing a patient conversation with payer to a conversation with a provider (particularly a physician) is a little like comparing conversations with your telephone company to a conversation with your pastor. They may both be informative, but one is slightly more trusted.
Providers “own” patient engagement
Providers (particularly physicians and nurse practitioners/nurse coordinators) truly are the owners of patient engagement. Individual providers (versus large provider entities) generally are trusted to do what is best for a patient, and are in a position to influence a patient toward behaviors that are more cost-effective. With particular reference to our risk-stratified targeted patients, the engagement steps are:
- Inform the patient about the plan of care
- Solicit input on who (other than the patient directly) is able to support the patient in staying on the plan
- Identify the specific tasks that are the patient (or the patient’s family) responsibility, and
- Confirm the actual “process controls” that will be used to confirm that the patient completed his/her tasks.
Some might note that the first three steps have been roughly similar since first practiced by Hippocrates. The new innovations are:
- The plan of care itself can now be much more detailed, and
- The “process controls” over compliance with the plan can now be significantly automated.
However, if you were thinking that the techniques for patient engagement were more art than science, wait until the next section.
What are “process controls” anyway?
Process controls are the techniques used to keep a process on an expected plan. Some people prefer the term “workflow” to process controls. In our view, “workflow” implies a task sequence but does not emphasize the alerts and back-up activities that underpin the compliance with a plan. We believe that the real value of contemporary technology is the capability to use process controls creatively to:
- Design plans of care that have patient/family tasks specifically identified (along with provider tasks)
- Delegate some fraction of the “back-up” activity to maintain compliance to the patient’s family, and
- Automate the patient’s compliance such that the provider is only involved if non-compliance is material.
Clearly, the greater the degree of patient engagement, the greater capacity for delegation of tasks onto the patient/family and the greater need for effective process controls. Delegation of tasks to a patient/family without structured patient engagement and without effective process controls is the technique Hippocrates used.
Hippocrates left practice before contemporary technology enabled effective process controls (and many contemporary physicians are debating the same career choice). But to discuss the use of technology, we have to move to the the “Virtualize Access” discussion here:
Go to “Virtualize Access”



