How ought we target patients for “special” care management attention?
Generally, the process used to proactively identify patients for increased care management focus is called stratification. Much has been written, demonstrated, piloted and refuted with respect to the “best” approach. In the end, the process to stratify patient populations is a mix of art and science. The experience with population-based care management is not as pervasive as one might hope. This state-of nature is mostly due to the existence of that broadly-experienced evil: fee-for service medicine.
The virtue of “Accountable Care”
Many health systems have invested time, money and creativity in attempting to mitigate utilization for the highest utilizers. The efforts have been uneven across the US, however. This is mostly due to the lack of economic incentives on the part of provider organizations to spend money to decrease utilization (activity for which they are usually not compensated) when the result is a decrease in utilization (wherein providers lose revenue). The advent of more pervasive accountable care payment structures has begun to give provider organizations more incentives to directly address the utilization issues in the patient populations in their service areas.
Who are the highest utilizers now?
The usual approach to stratification starts with identifying the current high utilizers. Historical utilization is often a good predictor of future utilization, and is usually more reliable (as a surprise to some) than degree of morbidity. The question one might ask is how much utilization is “high”? There are many rules-of-thumb that characterize the disparity of utilization across a general population. It is often noted that:
- 5% of patients consume 45% of costs
- 45% of patients consume about 5% of costs, and
- The remaining 50% incur about 50%
For our purposes, the above numbers (although roughly true) are not particularly useful. A more useful cascade of utilization metrics is as follows (please allow for some license here- patient populations are different):
- The top 1.5% of patients incur about a third of care costs
- The top 5% incur about half care costs
- the top 50% incur about 95% of care costs
In our view, this characterization of the utilization spectrum give us an idea of what to do about it.
Different utilization, different care approach
We prefer to characterize the approach to care management based on the following:
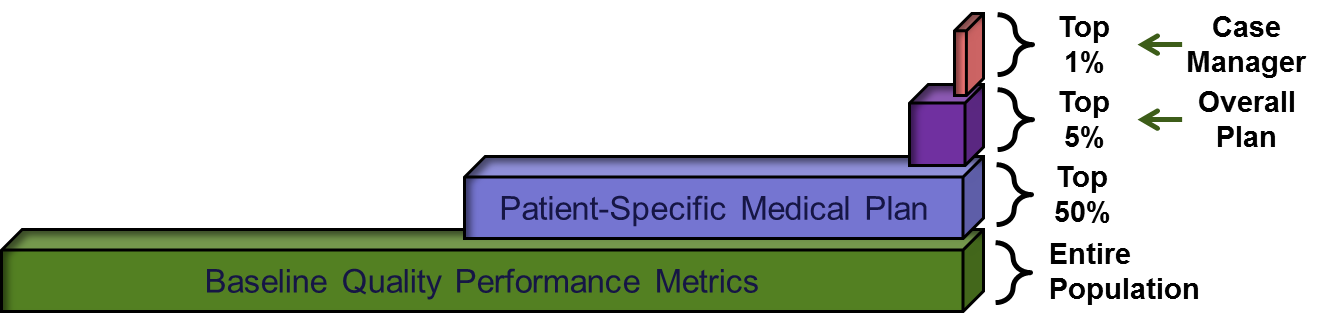
In this framework, we can see different types of care management plans based on the degree of utilization of the population. As patients incur higher utilization, they are greeted with an increase in the degree of care coordination offered by the provider organization. The plans are arranged roughly as follows:
- Full population: Apply all evidence-based medicine guidelines consistent with quality reporting and the best standards of medical practice
- Top half of utilizers: Add a patient-specific plan of care based on medical status (including functional status)
- Top 5%: Add an environmental and psycho-social assessment onto the medical plan, and include management of non-medical interventions into the plan of care, and
- Top 1%: Dedicate a portion of a case manager to the patient
The notion of the “top 5%” and “top 1%” should be considered as metaphorical. The top bracket is probably closer to 1.5%, and the next bracket is probably in the 3-6% range.
A word about tools
There are several vendors with tools that are effective at “predictive analytics” to stratify patients into risk groups. Although the tools can be powerful assistants, the real issue is deciding what to do with the output of the tools. Our team has worked with a variety of tools/vendors, and many of the analytic tools are very useful.
So, what do we actually do with these patients?
Now it is time to look at the “Plan Care” phase of the effort:
Go to “Plan Care”



